Custom Tailored Medical Billing Services Company
We have a 99.9% claim acceptance rate.
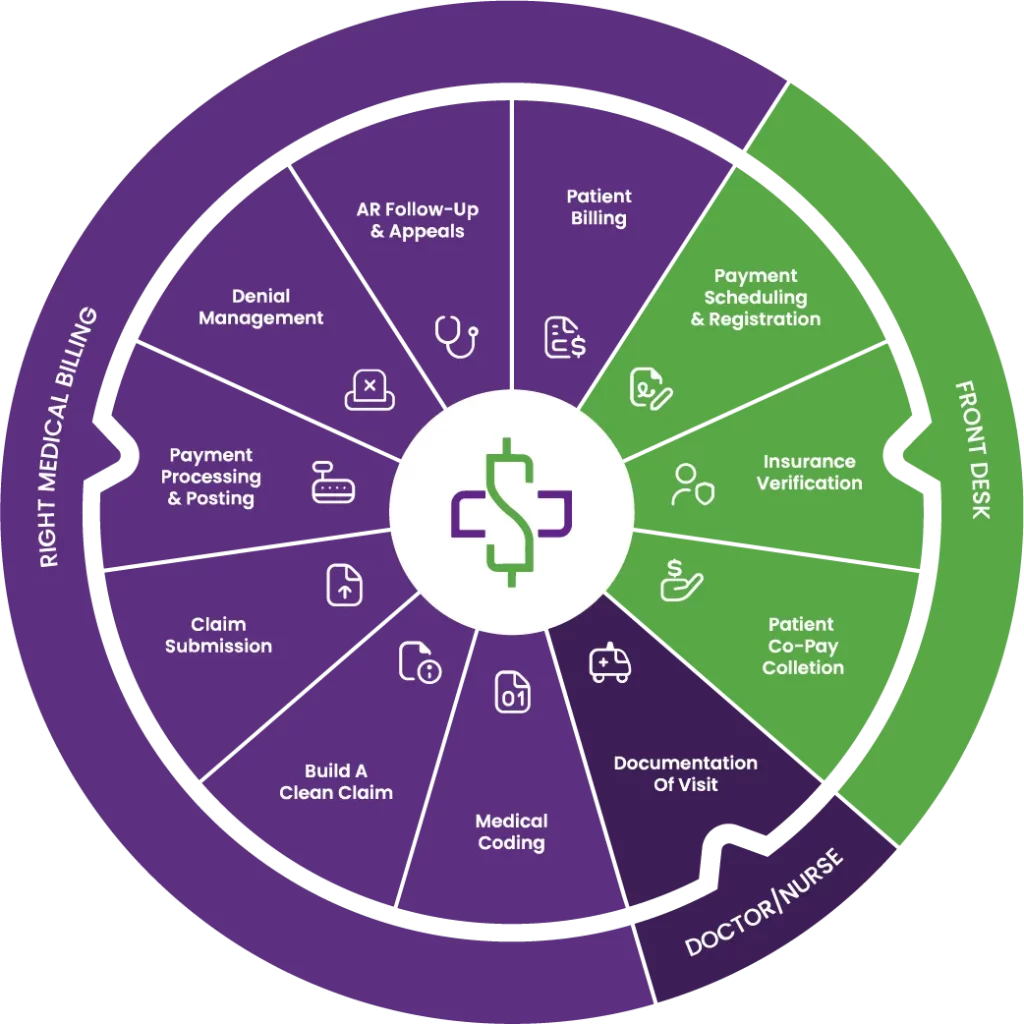
From the moment your patient walks in until you receive payment for the services rendered, our medical billing services team supports your growth by focusing on problem areas in your revenue cycle.

1200+ Providers Served
100+ Medical Specialties
500+ Certified Coders & Billers
50 States Served
Our Client Base
Right Medical Billing offers comprehensive medical billing and revenue cycle management services to a diverse client base. We partner with healthcare providers of all sizes, from solo practitioners navigating complex healthcare landscapes to large healthcare systems managing bustling operations. Our commitment lies in delivering tailored solutions that drive revenue and efficiency to your practice.
Why Choose RMB as your Medical Billing Services Provider?
As your dedicated medical billing services provider, we’re an extension of your practice. Imagine us as your financial team. While you focus on patient care, we’ll handle the complex world of insurance claims, patient billing, and revenue collection. Together, we'll ensure your practice runs smoothly and efficiently.
Your healthcare facility is a complex system with many moving parts, all working together to deliver exceptional patient care. We at Right Medical Billing are proud to be a vital component of that system. As a trusted medical billing services provider, we handle the financial aspects of your practice, allowing your team to focus on what they do best: providing compassionate care.
Medical Billing Services & Solutions that Streamline Your Revenue and Improve Your Cashflow
Medical Billing and Coding
The single most important element to guarantee reimbursements is proper medical billing and coding. Even the smallest mistake can result in a delay of payment. Right Medical Billing has a dedicated team of billers and coders that ensure patients and payers reimburse healthcare facilities for the services that they deliver.
Learn MoreAccounts Receivable Management
Right Medical Billing aggressively manages your practice’s accounts receivable by pinpointing any outstanding payments that the provider or healthcare facility should be expected to receive, then pursues the patient or insurance payer for the unpaid balance. We post payments in a timely manner to ensure an optimal billing process.
Learn MoreComplete RCM services
Right Medical Billing offers you complete revenue cycle management, starting from the moment your patient walks in the door up until the payment for your services are received. We are available to manage and educate your staff on compliance, streamlining workflow, and maximizing productivity. Think of us as an extension of your staff.
Learn MoreOut of Network Negotiation
Right Medical Billing negotiates out-of-network claims aggressively with pricing vendors such as Multiplan, Zelis, Viant, and GCS. Our negotiation and settlement team have decades of expertise. Out-of-network billing is the trickiest aspect of billing, and we are well-known in this industry as the experts in the field.
Learn MoreCredentialing & Contracting
Credentialing and contracting are the basis of starting a healthcare facility. They also lay the foundation for your relationships with insurance companies as well as patients. RMB will negotiate contracts with insurance payers and ensure that your contracts are up to date so you can attain the highest reimbursement rates.
Learn MoreBenefits of Choosing Our Medical Billing Services
Right Medical Billing will not only take care of your financial burdens, but we, as a company, will strive to improve your overall RCM operations. This is our promise to all of our medical billing clients across the US. Just as you are the best at what you do, we are the best at what we do. If you succeed, we succeed.
Below are some of the reasons as to why many of our clients decided to choose us over our competitors.

More Focus on Patient Care
Reduced Administrative Duties
Enhanced Cash Flow
Reduced Billing Errors
Improved Patient Satisfaction
Secured Patient Data
Billing Compliance
Process Claims Faster
Is Your Practice Leaving Money
on the Table?
Our expert audits carefully identify hidden revenue leaks caused by coding errors, patient demographic inaccuracies, and claim denials.
Maximize your reimbursements and streamline your billing process for optimal financial health.
Compliance Audits
- Ensure adherence to all applicable regulations including HIPAA, Medicare, and Medicaid.
- Verify coding accuracy to prevent claim denials and underpayments.
- Validate patient demographic information for accurate claim submissions.
- Review claim submission processes for timely and accurate filings.
- Assess payment posting accuracy to avoid errors and delays.
Revenue Cycle Audits
- Identify and address coding errors that impact reimbursement.
- Analyze claim denials to identify common causes and develop prevention strategies.
- Evaluate the efficiency of the billing process to identify bottlenecks and improve workflows.
- Review payment posting procedures for accuracy and timeliness.
- Assess the overall health of your revenue cycle to identify areas for improvement.
Internal Control Audits
- Evaluate the effectiveness of internal controls to prevent fraud and errors.
- Review access controls to ensure that only authorized personnel have access to sensitive data.
- Ensure that all necessary information is captured and retained carefully.
- Assess compliance program's effectiveness.
- Address potential conflicts of interest among employees.
Our Medical Billing Process
1. Provider Enrollment & Credentialing
Right Medical Billing completes payer enrollment and credentialing to ensure providers are approved and reimbursed without delays.
2. Patient Registration & Insurance Verification
We verify patient eligibility, benefits, and authorizations upfront to prevent rejections and payment issues.
3. Accurate Medical Coding
Certified coders assign precise ICD-10, CPT, and HCPCS codes, ensuring compliance and maximizing reimbursement.
4. Charge Entry & Claim Scrubbing
All charges are entered accurately and scrubbed using advanced tools to deliver clean claims.
5. Clean Claim Submission
Our Medical Billing Services ensure timely electronic claim submission for faster payer processing.
6. Payment Posting & Reconciliation
Payments, ERAs, and EOBs are posted accurately, with discrepancies identified quickly.
7. Denial Management & Appeals
Denied and underpaid claims are corrected and appealed aggressively to recover lost revenue.
8. Accounts Receivable Follow-Up
Dedicated AR specialists follow up consistently to reduce aging and improve cash flow.
9. Patient Billing & Support
Clear patient statements and responsive support enhance patient satisfaction and collections.
10. Reporting & Revenue Cycle Management Insights
RMB delivers transparent reporting and performance insights, ensuring complete Revenue Cycle Management and continuous improvement through expert Medical Billing Services.
Client Testimonials
-
"I want to extend my gratitude to the RMB billing team for their exceptional work. Your dedication, accuracy, and responsiveness have made a real difference, and the outstanding collections performance reflects your diligence and strategic approach. It’s clear you’ve taken true ownership with care and precision, and your work is both seen and deeply valued."
Dr. Kene EnekebeMemorial Spring ER -
"If you want full attention and knowledgeable expertise on the full revenue cycle management process, I highly recommend Right Medical Billing. We have seen a drastic improvement in our billing efficiency and collections since we outsourced billing to RMB. Humaira and her team are committed to putting in the work to collect all of your money."
 Zawadi BryantCEO Nightlight Pediatric Urgent Care - Houston, Texas
Zawadi BryantCEO Nightlight Pediatric Urgent Care - Houston, Texas -
"I transitioned into a private practice hence I did not have prior experience with medical billing or credentialing. RMB was an excellent choice for getting me credentialed with insurances. Humaira was always available for any questions I had. I am grateful to RMB and Humaira in helping me setup my practice."
 Dr. Niral PatelPhysician, Raynav Family Medicine
Dr. Niral PatelPhysician, Raynav Family Medicine -
"The RMB billers are highly knowledgeable and very pleasant. I highly recommend RMB. They have done a fantastic job for us. I strongly recommend RMB to anyone who wants to enjoy excellent customer service and more revenue!"
 Kumar GoswamiDow Healthcare Inc. - Director of Operations
Kumar GoswamiDow Healthcare Inc. - Director of Operations








