How to Effectively Review Your Revenue Cycle Process?
Healthcare businesses are no newcomers to insurance claim reimbursements being postponed or refused. Because it is believed that about 25% of denied claims are never reimbursed at all, practices dealing with this problem are at a high chance of losing revenue throughout the year. If your firm’s rejection rates are exceptionally high, this is an issue that must be addressed and handled so that your practice can continue to treat clients and generate money.
Among the most successful tactics to identify how to avoid such rejections is to examine and analyze your practice’s revenue cycle. Let’s understand how to perform this sort of evaluation and how right medical billing solutions may assist you in optimizing your revenue cycle for practice growth.
Why Is Insurance Claim Being Denied?
According to MGMA statistics from 2019, there are several typical reasons why insurance claim payouts are refused. The most common reason is a lack of stats or inaccurate information, such as demographic data, procedure codes, or diagnostic codes. Prior authorization is not being carried out in a similar idea.
Other typical reasons for claim rejections include failure to meet medical necessity criteria, treatments not being paid (eligibility problems), payer processing mistakes, the practitioner being out of the community, and benefits integration.
Rejections are a problem for healthcare practitioners since they can result in lost income and payment and force the billing team to analyze and resubmit the request. Rejection rates can be significantly reduced by analyzing a practice’s revenue cycle.
How to Evaluate Your Revenue Cycle Process Effectively?
A thorough revenue cycle analysis will assist your practice in avoiding claim rejections and ensuring that you get regular compensation for services rendered. The most significant advantages of decreasing denials for your business are greater profitability. Your revenue cycle analysis should involve a look at the following components.
1. Major Performance Metrics
To properly comprehend your revenue cycle, you must be well-versed in your practice’s key performance metrics. Once these have been identified, consider net recycling rate, days in account receivables, and other performance measures compared to industry best practices. This sort of study will help your approach to discover areas for development in the future.
2. Current Revenue Cycle Processes
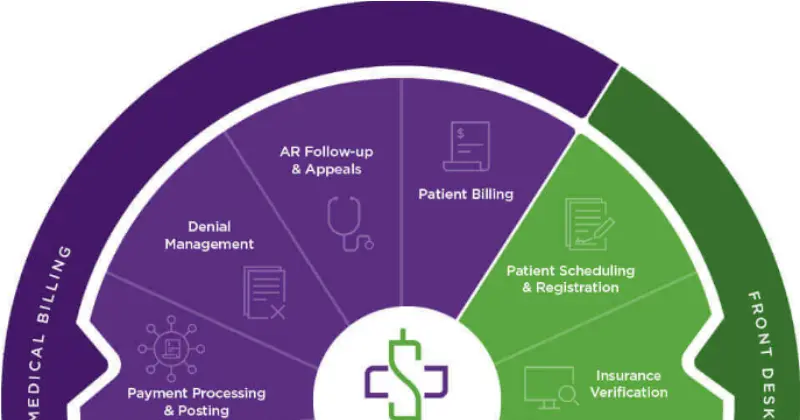
When analyzing your billing process, you should also focus on the process itself. Your revenue cycle is complicated, beginning with the registration process and concluding with insurance follow-up. Analyzing the process and its duration in completing each step of the process will help you identify opportunities for improvement by looking at the process from beginning to end.
3. Applied Revenue Cycle Resources
The use of particular technologies is certainly a part of your profession’s revenue cycle. Along the route, you should invest time in identifying which materials and resources are used for each activity. Please discuss how your team thinks about how the procedure is handled and which resources are most useful to them.
4. Staffing Plans
Your plans should also assess your firm’s workforce levels. Examine procedures with your team and establish the people required for each stage of the process and how much time is spent affected by variables such as specialty, patient information, and needed technology. You may also use this opportunity to handle any future personnel demands that may arise due to your new goals.
How We Can Improve Your Revenue Cycle Process
A thorough evaluation of your revenue cycle may significantly reduce the number of insurance claim rejections in your practice, resulting in higher income and overall practice efficiency. Right Medical Billing team specializes in revenue cycle management for medical billing and emergency room practices, and we would be glad to collaborate with you to help you succeed.
Our RCM services seek to reduce delivery time, prevent refiling expenses and reimbursement waits, and maximize cash flow. Right Medical Billing team especially try to conduct an expert opinion for your practice, allowing you to get ideas into what needs to be addressed and make the required adjustments moving ahead.
We are pleased to provide a wide range of practice management services to boost your practice to the top of your industry. Please get in touch with us immediately to learn more about what we have to offer.




