Predictive Analytics in AR Management: How Data Will Eliminate Denials Before They Happen
Accounts Receivable (AR) management is the financial backbone of every healthcare practice. Whether it’s a hospital, urgent care center, or private physician’s office, the ability to recover payments efficiently can define the sustainability of operations. Yet, one of the most persistent challenges practices face is claim denials—delays and losses that hurt cash flow and increase administrative burdens.
Traditionally, AR teams have relied on manual tracking, periodic audits, and after-the-fact appeal strategies to manage denials. But as the healthcare ecosystem becomes more complex, these reactive approaches are no longer sufficient. This is where predictive analytics—a data-driven, forward-looking technology—emerges as a transformative solution. By analyzing patterns in claims, payor requirements, and patient data, predictive analytics has the potential to eliminate denials before they ever happen.
In this blog, we’ll explore how predictive analytics is reshaping AR management, the benefits it offers, real-world applications, and why now is the right time for healthcare organizations to adopt it.
Understanding Predictive Analytics in AR Management
Predictive analytics uses statistical algorithms, artificial intelligence (AI), and machine learning (ML) models to examine large datasets, identify trends, and forecast outcomes. In the context of AR management, it means evaluating claim submissions, patient eligibility data, coding practices, and payer history to predict which claims are at risk of denial—before they are even submitted.
Instead of reacting to denials after they occur, predictive models empower billing teams to proactively correct errors, optimize documentation, and strengthen payer communication.
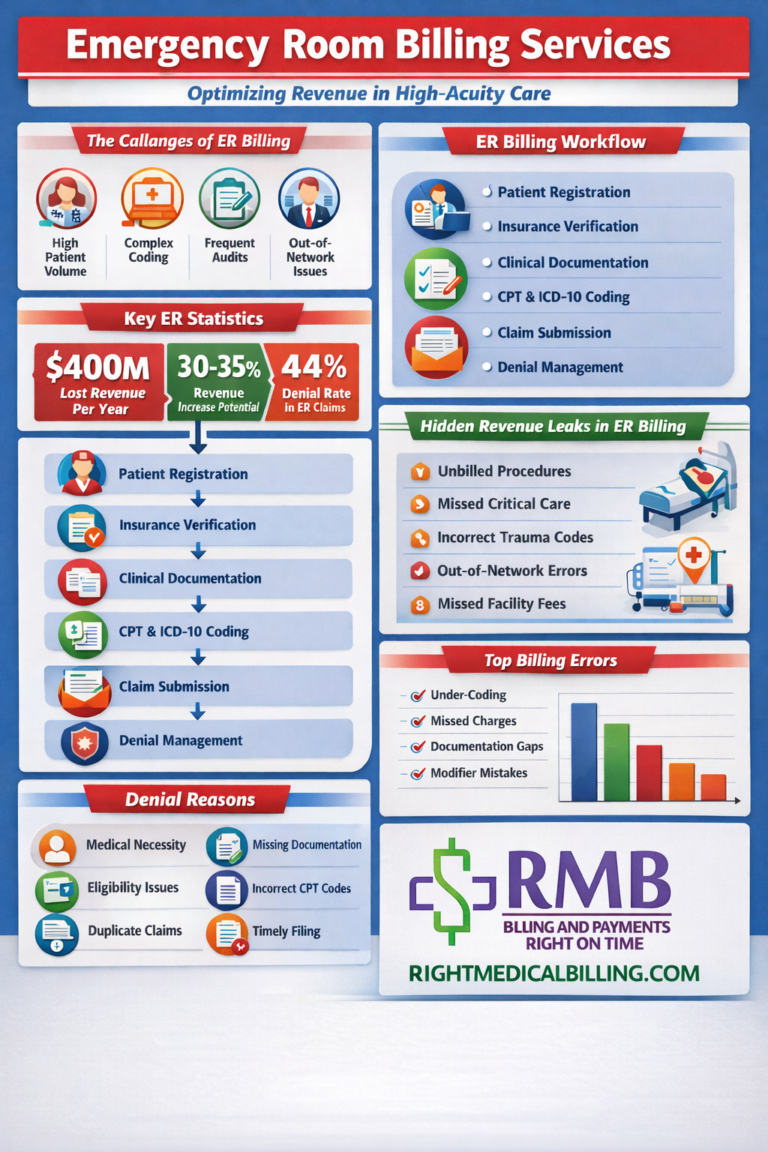
Why Denials Happen: A Data-Driven Problem
Before understanding how predictive analytics prevents denials, it’s important to see why they occur in the first place. The most common causes include:
-
Eligibility and Coverage Issues – Patients not covered at the time of service or incomplete insurance verification.
-
Coding Errors – Inaccurate CPT, ICD-10, or modifier usage.
-
Missing or Incomplete Documentation – Lack of supporting medical records or incomplete prior authorization.
-
Timely Filing Issues – Claims not submitted within the payer’s time limits.
-
Duplicate Claims – Multiple claims submitted for the same service.
-
Policy or Contractual Non-Compliance – Submitting services not covered under the payer contract.
Each of these errors is traceable and, more importantly, predictable with the right data inputs.
How Predictive Analytics Eliminates Denials
Predictive analytics transforms denial prevention from a manual guessing game into a structured, data-driven process. Here’s how it works:
1. Identifying High-Risk Claims Before Submission
Algorithms review historical claim data to flag claims that resemble past denials. For example, if a payer frequently denies certain CPT codes without supporting documentation, the system alerts the billing team before submission.
2. Real-Time Eligibility Verification
By integrating predictive tools with patient scheduling systems, providers can validate insurance coverage in real-time. Predictive models forecast potential eligibility mismatches, reducing the likelihood of coverage-related denials.
3. Error Pattern Recognition
Machine learning can detect recurring errors in coding and documentation. This allows billing teams to proactively train staff and correct systemic issues instead of repeatedly facing denials.
4. Prior Authorization Forecasting
Predictive models assess payer rules and identify services most likely to require prior authorization. By flagging these early, AR teams can avoid costly delays.
5. Optimizing Payer Communication
Analytics can map payer-specific denial trends and customize claim submissions to meet their unique requirements, improving first-pass acceptance rates.
The Benefits of Predictive Analytics in AR
When implemented correctly, predictive analytics doesn’t just reduce denials—it reshapes the entire AR ecosystem. Key benefits include:
-
Higher First-Pass Claim Acceptance Rates – Fewer claims bounce back, accelerating revenue cycles.
-
Reduced Administrative Costs – Less time spent on rework and appeals.
-
Improved Cash Flow – Faster reimbursements stabilize operational budgets.
-
Better Resource Allocation – Staff focus shifts from denial management to proactive claim optimization.
-
Enhanced Compliance – By aligning with payer rules and regulatory changes in real-time.
-
Informed Decision-Making – Leadership gains actionable insights on trends, improving strategic planning.
Real-World Application: A Hospital Case Example
Consider a mid-sized hospital struggling with a 20% denial rate. By integrating predictive analytics into its AR system, the hospital analyzed three years of claim history and payer trends. The predictive model flagged claims with high denial probability, particularly in emergency services and cardiology procedures.
By addressing documentation gaps, ensuring real-time eligibility checks, and training coders on common mistakes, the hospital achieved a 40% reduction in denials within six months. This translated into millions of dollars in recovered revenue and freed up administrative teams for other essential tasks.
Challenges and Considerations
While predictive analytics is a powerful tool, organizations must prepare for certain challenges:
-
Data Quality – Inaccurate or incomplete data will undermine predictive models.
-
Integration with Legacy Systems – Older billing platforms may need upgrades to handle advanced analytics.
-
Change Management – Staff must be trained to trust and act on predictive insights.
-
Initial Investment – Implementation costs may seem high, but the ROI justifies them in the long run.
The Future of AR Management with Predictive Analytics
As value-based care models expand, the pressure to minimize financial inefficiencies grows. Predictive analytics will increasingly become a standard feature in AR management, not a luxury. Future advancements may include:
-
AI-driven denial appeal automation – Systems that draft appeal letters automatically.
-
Dynamic payer rule libraries – Continuously updated databases of payer-specific requirements.
-
Predictive staffing models – Forecasting AR team needs based on expected claim volumes and payer behaviors.
Healthcare organizations that embrace predictive analytics now will be far ahead in the coming decade, securing financial health and operational stability.
Final Takeaway
Predictive analytics is not just about crunching numbers—it’s about transforming AR management into a proactive, intelligent, and denial-resistant system. By leveraging data to predict and prevent denials before they occur, healthcare providers can improve cash flow, reduce administrative strain, and ensure financial sustainability.
The future of AR management lies in moving from reaction to prevention, and predictive analytics is the bridge that makes it possible. Healthcare organizations that invest in this technology today will reap the benefits of smoother revenue cycles, fewer denials, and a stronger bottom line tomorrow.